Herniated discs, often referred to as slipped discs, are a common cause of back or neck pain that can make day-to-day activities—like bending, walking, or even sitting—challenging. The good news? With the right herniated disc treatment and approach, many individuals can manage their symptoms, regain mobility, and return to their normal routines over time.
Key Takeaways
- A herniated disc occurs when a spinal disc protrudes and irritates nearby nerves, often leading to back pain, numbness, or radiating symptoms.
- Most people recover well with conservative herniated disc treatment, which may include rest, medication, and structured physiotherapy.
- Recovery typically progresses in stages—from pain management and gentle movement to strength-building and injury prevention. Home physiotherapy can play a crucial role in this process.
- Key strategies like maintaining good posture, strengthening core muscles, and staying active with low-impact exercise can support long-term spinal health and prevent future injuries.
In this guide, we will walk you through what a herniated disc is, how recovery typically progresses, and practical tips for managing symptoms at home through physiotherapy.
Understanding Herniated Discs and Treatment Options
What is a Herniated Disc?
A herniated disc occurs when the intervertebral disc—the soft, gel-like cushion located between each vertebra—becomes displaced. These discs act as shock absorbers, protecting the spine during movement. Over time, or after an injury, the outer layer of the disc may weaken or tear, causing the intervertebral disc to protrude or leak out.
What Causes a Herniated Disc?
The most common cause of disc herniation is gradual wear and tear over time, also known as disc degeneration. As we grow older, the intervertebral discs in our spine gradually lose flexibility and strength. This makes them more prone to tearing or rupturing, even during everyday movements.
However, herniated discs can also be triggered or worsened by other contributing factors, such as:
- Poor posture from prolonged sitting or slouching
- Repetitive bending or twisting
- Lifting heavy objects with improper form
- Sudden trauma, such as a fall or accident
- Excess body weight, which may place additional strain on the spine
In many cases, it is a combination of these factors—rather than a single incident—that gradually weakens the disc over time.
Symptoms of a Herniated Disc

In some cases, the herniation may not present with any noticeable symptoms. However, when the protrusion presses on neighbouring nerves in the spinal canal, it can lead to a variety of symptoms depending on the location. For example:
-
Cervical spine (neck):
May cause neck pain, stiffness, and radiating discomfort, numbness, or tingling in the shoulder, arm, or fingers.
-
Lumbar spine (lower back):
Often results in lower back pain, shooting pain down the leg (sciatica), and possible numbness or weakness in the foot.
-
Thoracic spine (upper back):
Less common, but may cause pain radiating around the chest or abdomen, especially when twisting or breathing deeply.
Symptoms often fluctuate throughout the day. For example, many individuals find their pain intensifies in the morning due to overnight stiffness or after long periods of inactivity.
How It Affects Daily Life
Living with a herniated disc often means adjusting your daily activities because of pain or stiffness. Common challenges include:
-
Bending and lifting:
These actions place direct strain on the affected disc, often aggravating pain or triggering muscle spasms—especially if done without proper technique.
-
Prolonged sitting or standing:
Remaining in one position for too long increases pressure on the spine, which can lead to stiffness, discomfort, or a gradual build-up of pain.
-
Sleeping:
Finding a comfortable sleeping position may become difficult. Poor spinal alignment at night can worsen symptoms or cause morning stiffness, disrupting both rest and recovery.
Do You Need Surgery for a Herniated Disc?

While the term “slipped disc” might sound alarming, studies show that most herniated disc cases do not need surgical treatment. In many cases, symptoms resolve on their own within about six weeks with conservative care, which includes:
-
Activity modification:
Avoiding painful movements and finding ways to stay gently active, such as walking or gentle stretching.
-
Medication:
Doctors may prescribe anti-inflammatory drugs or muscle relaxants to manage symptoms temporarily.
-
Structured physiotherapy:
A physiotherapist can provide targeted exercises that support spinal alignment, reduce nerve pressure, and build core strength.
-
Lifestyle changes:
Reducing sedentary time, improving posture, and optimising daily ergonomics—such as using lumbar cushions or sit-stand desks—can reduce the strain on your back.
However, there are specific clinical red flags that may prompt surgical evaluation, including:
- Sudden or worsening muscle weakness
- Numbness or reduced sensation
- Loss of bladder or bowel control
- Persistent, severe pain (that does not improve after 6 to 12 weeks of physiotherapy and other conservative herniated disc treatments).
In such cases, surgical procedures such as microdiscectomy or spinal decompression may be considered to relieve nerve compression and address persistent symptoms.
However, even if surgical herniated disc treatments are recommended, post-surgical rehab is often an important part of the recovery process. Physiotherapists can help patients regain their strength, restore movement patterns, and reduce the risk of further complications.
Navigating Herniated Disc Treatment: Exercises, Progress, and Prevention

With a clearer understanding of what a herniated disc is and the treatment options available, the next step is to explore how recovery can start. In this section, we will walk you through what to expect during each stage of healing, how home physiotherapy supports progress, and practical tips for preventing future injuries.
Key Stages of Recovery and What to Expect
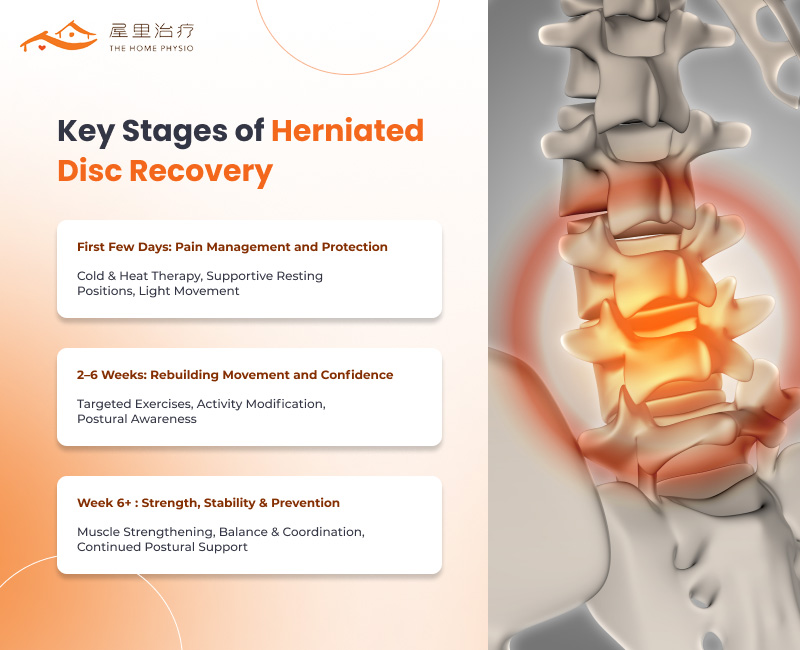
Recovering from a slipped disc is a gradual process that unfolds in phases. Each stage of recovery comes with its own focus and involves different conservative herniated disc treatments—ranging from pain management and guided movement to strength-building and long-term injury prevention.
First Few Days: Pain Management and Protection
In the initial phase following diagnosis, the primary goal of herniated disc treatment is to reduce pain and inflammation while protecting the affected area from further strain. At this stage, rest is important, but complete immobility should be avoided, as it can lead to stiffness and delayed recovery.
The following techniques may be incorporated into your herniated disc treatment plan:
- Cold and heat therapy: Applying ice packs during the first 48 hours can help reduce inflammation and numb acute pain. After the initial phase, heat may be used to relax tight muscles and alleviate tension caused by protective postures. Your doctor can guide you on when and how to alternate between cold and heat based on your symptoms.
- Supportive resting positions: Finding a comfortable position is key to reducing pressure on the spine. Using pillows or cushions to support the lower back, neck, or knees can make resting and sleeping more manageable. Your physiotherapist may also recommend specific techniques to help you get in and out of bed safely or reposition yourself without straining the injured area.
- Light movement: While avoiding strenuous activity is important, short walks around your home or neighbourhood can encourage blood flow and prevent joint stiffness. Gentle stretching, guided by a trained physiotherapist, may also be introduced to maintain spinal mobility and ease muscle tightness.
This is where home physiotherapy can play an important role, providing guidance and support in a familiar environment. A physiotherapist can assess your home setup, recommend safe strategies, and adapt early-stage care based on your individual needs. This approach can be particularly beneficial for patients who may find travel challenging during recovery.
2–6 Weeks: Rebuilding Movement and Confidence
As pain levels start to ease, the focus of herniated disc treatment shifts toward restoring movement, flexibility, and daily function. During this stage, physiotherapy becomes more active, helping you regain confidence in your movements without disrupting the healing process.
- Targeted exercises: Your home physio sessions may begin incorporating gentle, low-impact movements such as pelvic tilts, knee rolls, or supported spinal stretches. These exercises are designed to restore flexibility, engage the core, and support alignment without placing excess strain on the spine.
- Activity modification: Although pain may have decreased, it is important to avoid sudden bending, twisting, or lifting—these can still aggravate the healing disc. A physiotherapist can guide you in adjusting daily tasks—like getting dressed, lifting light objects, or doing housework—using safe movement practices.
- Postural awareness: Maintaining a neutral spine throughout the day becomes a priority. Sitting with proper back support, standing with even weight distribution, and avoiding slouched positions can help relieve pressure on the affected area.
Week 6 and After: Strengthening, Stability, and Long-Term Prevention

As recovery progresses past the six-week mark, herniated disc treatment shifts toward restoring strength, enhancing stability, and reducing the risk of future flare-ups.
Key components of this phase typically include:
- Progressive strengthening exercises: Your physiotherapist may introduce more challenging movements to reinforce proper spinal alignment and distribute pressure more evenly. In lumbar spine physiotherapy, for example, targeted core work is often used to support the lower back and improve trunk control. Depending on your progress, resistance bands or light weights may also be incorporated to support muscle endurance and functional strength.
- Balance and coordination training: Exercises like single-leg stands, heel-to-toe walking, or step-ups help retrain your body’s ability to respond to changes in position or terrain. These movements improve proprioception—your body’s awareness of space and movement—which helps prevent falls or awkward movements that could lead to re-injury.
- Continued postural support: Even at this stage, maintaining good posture remains important. Your physiotherapist can help you reinforce habits that support spinal health, especially during activities like lifting, prolonged sitting, or transitioning between tasks.
After Herniated Disc Treatment: Tips for Preventing Future Injuries
Once symptoms have stabilised, sustained recovery from a herniated disc also requires building habits that protect your long-term spinal health.
1. Practise Good Posture

Maintaining a neutral spine—whether you are sitting at your desk, standing in line, or lifting an object—can help distribute pressure more evenly and reduce pressure on your spine. Make simple adjustments, such as keeping your ear aligned with your shoulder and avoiding slouched positions.
2. Strengthen Your Core Muscles
Your core—which refers to the muscles around your abdomen and lower back—helps support your spine during day-to-day activities. Strengthening these muscles through targeted exercises like pelvic tilts, modified planks, and bridges can help enhance spinal stability and reduce the strain placed on your spinal structures. If you are still undergoing herniated disc treatment, your physiotherapist will adapt these exercises to your current strength and stage of recovery.
3. Use Safe Movement Techniques
Everyday actions such as bending, lifting, or reaching can place added stress on the spine, especially if performed with improper technique. To reduce strain, it is advisable to bend at the knees while keeping the back straight when lifting objects and to avoid twisting your spine, particularly when carrying weight. Practising safe movement habits can help minimise pressure on the discs and support safer, more efficient motion during daily tasks.
4. Prioritise Ergonomics at Home
Your physical environment has a big influence on your spinal health. Ensure that your chair provides lumbar support, your desk is at the correct height, and your mattress and pillow promote spinal alignment. These small ergonomic adjustments can help reduce the cumulative stress on your back throughout the day.
5. Keep Moving and Stay Active
Staying active is not only an important aspect of long-term herniated disc treatment but also plays a vital role in supporting your overall well-being. Regular exercise helps maintain joint flexibility, muscle strength, and circulation, which can help reduce the risk of stiffness and future strain.
Low-impact activities such as walking, swimming, or cycling can be gentle on the spine while keeping the body engaged. Aim to include some form of movement most days of the week—even 20 to 30 minutes a day can make a meaningful difference over time.
Frequently Asked Questions
1. What are some of the benefits of home physiotherapy when it comes to herniated disc treatment?
Home physiotherapy provides the convenience of receiving care in a familiar setting, which can be especially helpful for individuals experiencing pain or limited mobility. By eliminating the need to travel, it may also help reduce physical and mental stress during recovery. In addition, a home physiotherapist can monitor your recovery and tailor exercises to fit your daily routine and living space. This supports safer movement and greater consistency over time.
2. How can I help a loved one who is suffering from a herniated disc or chronic back pain?
You can support your loved one by creating a safe and comfortable environment for their recovery. For example, assist with tasks that may strain their back, such as lifting heavy items around the house, and encourage them to stay consistent with their prescribed exercises. Being present, patient, and understanding can go a long way.
3. Can I do my physiotherapy exercises on my own?
As part of a comprehensive herniated disc treatment plan, a physiotherapist can develop a personalised exercise plan and demonstrate techniques intended to minimise strain during movement. While it is important to continue these exercises regularly at home, periodic check-ins are important for reviewing your form, monitoring your response to the exercises, and adjusting the programme based on your progress.
Supporting Your Recovery With Home-Based Herniated Disc Treatment
Recovering from a herniated disc is a journey that calls for patience, consistent effort, and an emphasis on safe movement. With the right approach, many individuals are able to manage symptoms effectively and return to their daily routines with greater confidence.
If you are looking for herniated disc treatment in the comfort of your home, The Home Physio provides personalised, evidence-informed care right where you live. From comprehensive physio spine services to guided neurological rehabilitation and geriatric care, we tailor each treatment plan to meet your individual needs.
Let us work together on your recovery—contact us to learn more.

